In this post I link to and excerpt from the chapter Hyponatremia, December 12, 2019, of Dr. Farkas’ incredible Internet Book Of Critical Care [Link is to TOC]. And after reviewing the chapter, listen to the wonderful 35 minute summary podcast of the chapter. At least that is the order that seems to work best for me.
Dr. Farkas has created this Table of Contents of the chapter and each heading is a direct link to that part of the chapter! Awesome.
CONTENTS
- Diagnosis
- Causes
- Evaluation
- Risk stratification
- Initial treatment (e.g. in ED)
- Subsequent therapeutic strategy
- Oops, the patient’s sodium over-corrected
- Why not to use vaptans
- Algorithm
- Podcast
- Questions & discussion
- Pitfalls
- PDF of this chapter (or create customized PDF)
Here are excerpts from the hyponatremia chapter:
Pitfalls
- Don’t forget to implement free water restriction for all hyponatremic patients (at least early on, while the dust is settling).
- Don’t use vaptans. It’s that simple, just don’t use them.
- If you use the DDAVP clamp, be sure to restrict the patient’s fluid intake. The combination of DDAVP plus unrestricted fluid intake can worsen the patient’s hyponatremia.
- Patients with symptomatic hyponatremia should be treated with hypertonic fluid (either 3% saline or hypertonic sodium bicarbonate). Don’t use normal saline here, because if the patient has SIADH this may exacerbate their hyponatremia.
- If the patient’s sodium rises too quickly, don’t give up (“well the patient’s ok, they seem to have tolerated it”). Patients may look OK for a while, but later develop osmotic demyelination. If the patient’s sodium over-corrects, give them DDAVP and water, and reduce the sodium to the appropriate target.
Diagnosis
This is a lab diagnosis.
- Consider repeating the lab before initiating therapy, especially if it doesn’t match the clinical scenario or if other electrolytes are deranged. An aberrantly low sodium may result from drawing electrolytes upstream from a hypotonic infusion.
symptoms
- Severe
- Seizure
- Neurogenic pulmonary edema
- Delirium
- Non-severe
- Nausea, vomiting
- Headache
- Mild confusion
- Dizziness, gait instability
- Tremor, multifocal myoclonus
- Hyperreflexia, muscle cramps
Causes
pseudo-hyponatremia (serum osmolality is normal or low)
severe renal failure
rare scenarios with water intake > solute intake
hypovolemia
- Non-renal losses
- GI loss (vomiting, diarrhea, gastric tube drainage)
- Hemorrhage
- Sweating, burns
- Renal losses
- Diuretics (especially thiazides)
- Post-obstructive diuresis
- Cerebral salt wasting
- Hypoaldosteronism, adrenal insufficiency (late)
euvolemic hyponatremia
- Adrenal insufficiency (early)
- Hypothyroidism
- SIADH
- Medications (this list is incomplete; when in doubt evaluate the medication list using Medscape or Epocrates for possible causative agents).
- Vasopressin or DDAVP (these don’t technically stimulate ADH release, but rather directly stimulate ADH receptors.)
- NSAIDs
- Chemotherapy
- Psych (antipsychotics, SSRIs, tricyclics, MAO inhibitors)
- Carbamazepine, oxcarbazepine, valproate
- Oxytocin, bromocriptine
- Ecstasy (MDMA)
- Malignancy (especially small cell lung carcinoma)
- Neuropsychiatric disorder (virtually any)
- Pulmonary dysfunction, severe
- Pain or nausea (especially post-operative or due to extreme exercise)
edematous states (hypervolemic hyponatremia)
- Heart failure with low cardiac output
- Cirrhosis
- Nephrotic syndrome
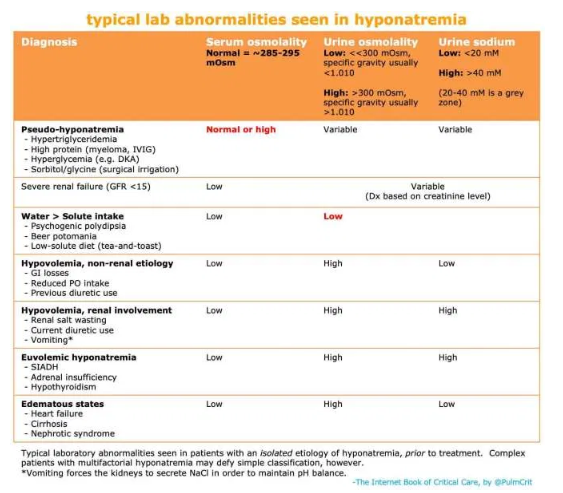
Lab Panel
serum labs
- Full set of electrolytes (including Ca/Mg/Phos) & glucose
- Serum osmolality
- Normal or increased level indicates pseudohyponatremia. This is an unusual finding, but is totally game-changing.
- Thyroid-stimulating hormone (TSH) & cortisol
urine osmolarity
- The preferred way to measure this is a direct measurement of urine osmolality. However, a crude estimate can be obtained by looking at the urine specific gravity. A specific gravity <1.010 suggests dilute urine, whereas a specific gravity >1.010 suggests concentrated urine (Imran 2010).
- Concentrated urine (urine osmolality >300 mOsm, specific gravity >1.010)
- Diagnostic significance
- Most hyponatremic patients will have a urine osmolality of >300 mOsm.
- This is nonspecific, revealing relatively little about the diagnosis.
- Therapeutic significance
- Concentrated urine indicates that the kidney is still retaining water. This indicates that the patient is not going to auto-correct their sodium.
- A very concentrated urine suggests that giving isotonic fluid could potentially worsen the hyponatremia (because the kidney may respond by retaining water and excreting sodium, a process termed “desalination”).
- Dilute urine (urine osmolality <<300 mOsm, specific gravity <1.010)
- Diagnostic significance:
- The kidney is secreting water – that’s what it’s supposed to do! The kidney is working correctly. This suggests one of the following situations:
- (1) Hyponatremia due to water intake >> solute intake (see purple differential above).
- (2) A patient in the recovery phase from any other cause of hyponatremia (e.g., the patient initially had hypovolemic hyponatremia, received volume resuscitation prior to urinalysis, and is currently auto-correcting their own sodium levels.)
- Therapeutic significance:
- Secretion of dilute urine will cause the patient’s sodium to rise – so these patients will correct their own sodium levels.
- Production of large volumes of dilute urine is often a sign that the sodium is about to over-correct.
urine sodium
- Low urine sodium (<20 mEq/L) suggests:
- Hypovolemic hyponatremia due to extra-renal volume loss.
- Hypervolemic hyponatemia (e.g. heart failure, cirrhosis).
- Intermediate urine sodium (~20-40 mEq/L)
- This represents a grey zone, provides no clear information.
- High urine sodium (>40 mEq/L) suggests:
- Euvolemic hyponatremia (SIADH, hypothyroidism, or adrenal insufficiency).
- Hypovolemic hyponatremia due to renal salt wasting (e.g. diuretics, vomiting, or cerebral salt wasting).
Diagnostic Strategy
Traditional Diagnostic Algorithms Often Fail Because:
- (1) Clinicians cannot reliably determine volume status at the bedside. We may be able to differentiate hypovolemia from hypervolemia, but the borderline between euvolemia vs. hypovolemia is often impossible to determine.
- (2) A single cutoff value for urinary sodium (20 mM) is used. Different sources disagree about what cutoff to use, so there seems to be a grey zone here.
- (3) In reality, the urine electrolytes often aren’t checked prior to administering fluid. Without a properly timed urine electrolyte measurement, the algorithm collapses entirely.
- (4) Patients often have multifactorial hyponatremia. Multifactorial disease will confound simple diagnostic algorithms.
a more reasonable approach
- Collect several key pieces of information:
- (1) Hyponatremia lab panel (the table above may help interpret the urine electrolytes).
- (2) Medication list & recent medication changes.
- (3) History of any recent precipitating events (focus on fluid balance, e.g. water intake, vomiting, diarrhea, exertion).
- (4) Physical examination of volume status (including ultrasonography).
- Synthesis of this information is generally sufficient to yield a diagnosis (or at least, a provisional diagnosis).
- Response to therapy will sometimes add diagnostic clarity, for example:
- Persistent, recurrent hyponatremia reflects an ongoing cause (e.g. chronic SIADH).
- Hyponatremia which is easy to correct and doesn’t recur suggests a transient cause (e.g. hypovolemia).
risk stratification
Generally speaking, there are two things to worry about with a patient with hyponatremia. First, hyponatremia may deteriorate or lead to severe complications (e.g. seizure, cerebral edema, and herniation). Second, hyponatremia may over-correct too fast, leading to osmotic demyelination. Both of these possibilities should be borne in mind when approaching the patient with hyponatremia.
risk for seizures/herniation due to hyponatremia
- (a) Symptoms of hyponatremia
- (b) Acute hyponatremia
- (c) Brain substrate
- Premenopausal women (little extra space in cranium for brain to swell)
- Intracranial pathology (e.g. space-occupying lesion, cerebral edema)
- Known seizure disorder
risk for osmotic demyelination syndrome due to rapid correction
- (a) Reversible cause of hyponatremia
- Hypovolemia, adrenal insufficiency
- SIADH due to a transient factor (e.g. pain, nausea, or medication)
- Situations where water intake > sodium intake (e.g. beer potomania, psychogenic polydipsia, tea-and-toast diets)
- (b) Chronicity & severity
- Severe, asymptomatic hyponatremia is the most worrisome (especially Na <110 mM)
- (c) Other risk factors for osmotic demyelination syndrome (30181129)
- Hypokalemia (more on hypokalemic hyponatremia below)
- Cirrhosis
- Alcoholism
- Malnutrition
key point: The malnourished, alcoholic patient will often have numerous risk factors for central pontine myelinolysis (hypokalemia, cirrhosis, alcoholism, and malnutrition).
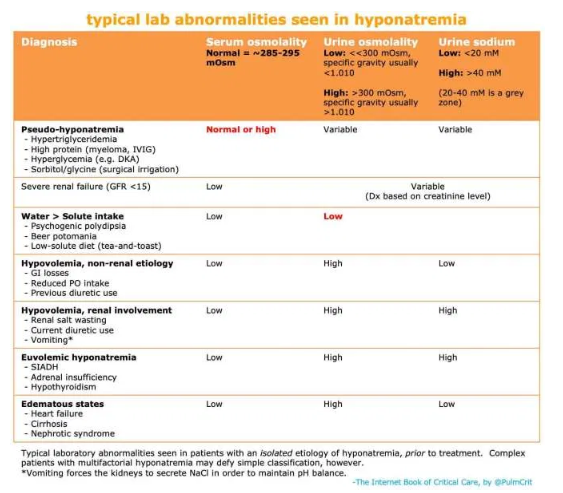
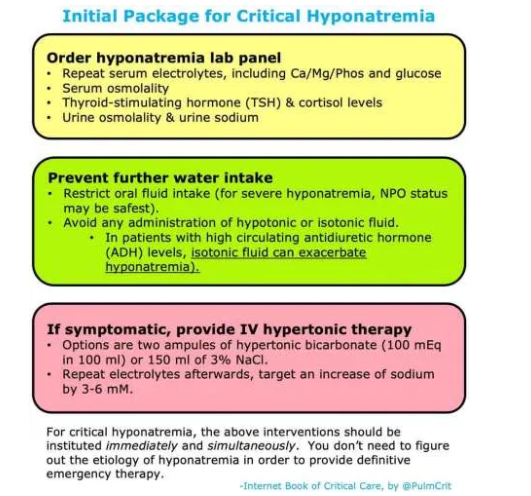
initial hyponatremia package
initial management
- Initial management is pretty simple, because the same management strategy can be applied regardless of the cause.
- Fire off the hyponatremia lab panel (don’t waste a lot of neurons on exactly which tests to get, just order them all and keep moving).
- Don’t delay therapy while waiting for these labs to come back. These labs are not needed for immediate treatment of hyponatremia.
- Stop further intake of free water (including isotonic fluids).
- As explored above, isotonic fluids are potentially dangerous in patients with hyponatremia!
- The only decision to be made here is whether to give hypertonic therapy, explored in the next section:
initial hypertonic bolus PRN
indicated in symptomatic hyponatremia, e.g.:
- Seizure
- Confusion
- Headache, nausea, vomiting
- Dizziness, gait instability, tremor, multifocal myoclonus
clinical context is more important than the numeric value of sodium, for example:
- Young woman with acute hyponatremia, Na of 125 mM, nausea and headache: This is an emergency, give hypertonic therapy immediately.
- Elderly man with chronic hyponatremia, Na of 125 mM, asymptomatic: This might not even warrant hospital admission, don’t get too excited about it.
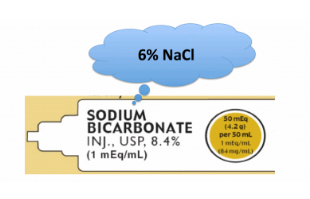
tx option #1 = hypertonic bicarbonate
- Hypertonic bicarbonate is defined here as 1 mEq/ml sodium bicarbonate, which is generally found in ampules of bicarbonate in crash carts.
- This solution of 1 mEq/ml sodium bicarbonate has the same tonicity as would 6% NaCl.
- In the United States, each hypertonic bicarbonate ampule generally contains 50 ml (as shown above).
- Hypertonic bicarbonate is usually the fastest medication to obtain in an emergency.
- A typical dose is two ampules (100ml) of hypertonic bicarbonate (equivalent to giving ~200 ml of 3% saline, which will raise the serum sodium by ~3 mM). For smaller patients, 1 or 1.5 ampules (50-75 ml) might be more appropriate (depending also on the clinical context and the urgency of increasing the sodium).
- Ampules of bicarbonate should generally be infused slowly (e.g. each one over 5-10 minutes). Bicarbonate is contraindicated in patients with metabolic alkalosis, which would be exacerbated by the bicarbonate.
- More on this strategy here.
follow-up repeat electrolytes
- Repeat a full electrolyte panel after administration of hypertonic therapy.
- The goal is to increase the Na by about 3-5 mM, which should cause clinical improvement.
- If symptoms persist:
- If the sodium has increased by <4 mM, then an additional round of hypertonic therapy may be needed (with a goal of increasing the sodium by ~4-6 mM total).
- If the sodium has increased by 6 mM and the symptoms have not resolved, then hyponatremia isn’t the cause of the patient’s symptoms. Evaluate further for alternative or additional problems.
target rate of increase
target rates of sodium correction
- Target increasing the sodium by 6 mEq/L every 24 hours (and no more than 8 mEq/L). Note that if the sodium was increased by 4-6 mM acutely, this is included within the 6 mM increase which is desired over the first 24 hours.
- For example: If you raise the sodium by 6 mM to treat symptomatic hyponatremia, the goal over the next 24 hours is to maintain the sodium at that same level without any further rise.
- Excessively rapid correction runs a risk of osmotic demyelination. This is extremely debilitating and won’t be obvious immediately – hence the importance of controlling the rise in sodium.
- The key is the net rate of correction – so, if the sodium corrects too rapidly but then you re-lower the sodium, that’s OK.
- For patients with acute hyponatremia (definitely developing over <<48 hours), faster rates of sodium correction may be safe.
the physiology of sodium over-correction
- Over-correcting the sodium is almost never due to the practitioner’s giving too much sodium chloride.
- Common causes of over-correction:
- 1) The underlying cause of hyponatremia is reversed. This causes the body to suddenly excrete a lot of free water, thereby causing the sodium to rise. This form of auto-correction is by far the most common cause of over-correction. The DDAVP clamp may be used to avoid this pitfall (next section).
- 2) KCl administration, without taking into account the effect this will have on sodium (more on this below).
- 3) Treatment of hyponatremia with vaptans (more on this below).
- Note, also, that over-correction is easily treated if it occurs (more on this below). Patients who over-correct will do fine if their sodium is immediately re-lowered. The patients who develop osmotic demyelination are patients who over-correct and nothing is done about it.
use caution with predictive equations
[If] rapidly reversible cause – [Use the] DDAVP clamp
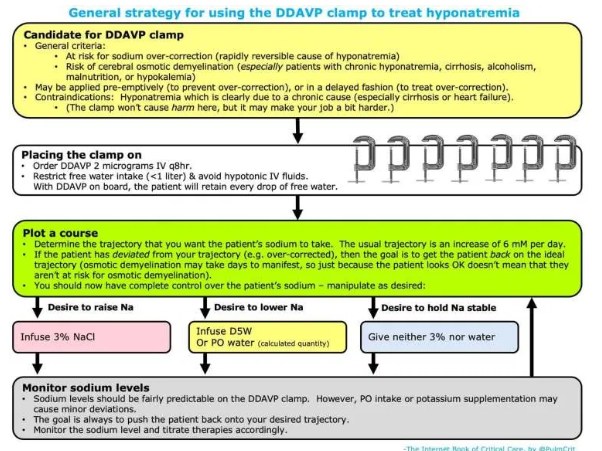
general concept
- This section discusses management of situations where the main concern is over-correction of the sodium, leading to osmotic demyelination.
- Risk factors for sodium over-correction & osmotic demyelination are listed above.
- The DDAVP clamp technique can be useful in patients at high risk for over-correction, or in patients who have already started to over-correct.
general concept of the DDAVP clamp
- Administration of DDAVP prevents the kidneys from secreting free water. This takes the patient’s kidneys out of the equation, preventing the patient from auto-correcting. The patient essentially becomes like a passive container, with very predictable behavior:
- Administration of hypotonic fluid (e.g. water, juice) will cause the sodium to decrease.
- Administration of hypertonic fluids (e.g. 3% saline, potassium tablets) will cause the sodium to increase.
- If there are no inputs, the sodium should stay roughly stable.
how to perform the DDAVP clamp
- Give DDAVP 2 micrograms IV q8 hours scheduled.
- The patient’s fluid intake must be strictly controlled.
- With DDAVP, if the patient drinks too much they will lower their sodium.
- To begin with, restrict any fluid intake (dry foods are OK). After 6-12 hours you may liberalize a bit.
- Note that the patient’s sense of thirst is due to hyponatremia, so there is no safe way to get rid of this immediately.
- Calculate the rate of 3% saline required to achieve your target sodium.
- Figure out how much more you want the sodium to increase over the next 24 hours.
- The effect of 3% sodium on your patient’s sodium can be calculated using this MDCalc equation.
- Infuse 3% saline via a peripheral vein (you don’t need a central line; 3% saline is safe for peripheral administration).
- Follow electrolytes every 4-6 hours to ensure that the sodium is on track.
- If the sodium is too low, increase the rate of 3% saline.
- If the sodium is too high, calculate the amount of free water required to decrease it back to target using this formula. This volume of free water may be given intravenously (as D5W) or orally (if the patient is able to drink).
- This is tedious, but effective.
removing the DDAVP clamp
- Once the sodium is close to normal (e.g. >125 mM), the DDAVP clamp may be discontinued. About 10 hours later, the patient’s diet may be gradually liberalized.
- One of two things will happen at this point:
- (a) If the cause of hyponatremia has been eliminated (e.g. hypovolemia), then the sodium will rapidly increase to normal and stay within a normal range. You’re all set.
- (b) If the patient still has a cause for hyponatremia (e.g. chronic SIADH), their sodium may start falling again. At this point, they would require maintenance therapy for SIADH (e.g. furosemide and oral salt tabs, or oral urea).
More information on the DDAVP clamp is located here.
SIADH with persistent cause
This section describes treatment of SIADH with an ongoing cause which is difficult or impossible to remove (e.g. malignancy, severe brain injury, or medications). Always be sure to look for all potential reversible causes of SIADH (e.g. medications listed above, nausea).
There are two preferred treatment strategies for chronic SIADH: oral urea or loop diuretic plus sodium.
[See this section of Dr. Farkas’ post for details]
heart failure
general comments
- Heart failure rarely causes profound hyponatremia. Rather, there is usually a fairly stable sodium of ~120-135 mM.
- Hyponatremia due to heart failure is usually chronic and is not a life-threatening process.
- Exactly when treatment is beneficial is unclear. The best approach to chronic, asymptomatic hyponatremia is often to provide no specific therapy for the hyponatremia. Instead, the primary focus of therapy should remain the heart failure.
- There is a risk of focusing too much energy on treating the hyponatremia, and not enough energy on treating the underlying heart failure. For example: It’s counter-productive for a cardiology service to refuse admission of a heart failure patient solely due to moderate hyponatremia.
cirrhosis
general comments
- Cirrhosis rarely causes severe hyponatremia. Similar to heart failure, there is usually a fairly stable sodium of ~120-135 mM.
- This is usually chronic and not a life-threatening process.
- Exactly when treatment is beneficial is unclear. The best approach to chronic, asymptomatic hyponatremia could be to do nothing.
treatment
[For details, see this section of Dr. Farkas’ post.]
hypokalemic hyponatremia
potassium increases tonicity as much as sodium does
- Administration of KCl will increase the sodium concentration just as much as NaCl would (they have the same impact on tonicity).
- This is a bit counterintuitive, because the potassium levels don’t increase much. However, potassium entry into cells is paired with the exit of sodium, such that the sodium levels will rise.
- 50 mEq of oral KCl will have about the same effect as 100 ml of 3% NaCl.
- The effect of intravenous forms of potassium will depend on exactly how they are formulated.
estimating the effect of oral KCl supplementation on serum sodium
[See this section of Dr. Farkas’ chapter for details.]
clinical significance
- Oral repletion of KCl will have a greater impact on serum sodium than we generally recognize. This should be accounted for in patients with significant hypokalemia.
- Failure to consider the osmotic effect of KCl is one driver of unexpected over-correction of hyponatremia.
- In some patients with moderate hyponatremia and moderate hypokalemia, oral repletion of KCl will simultaneously address both problems.
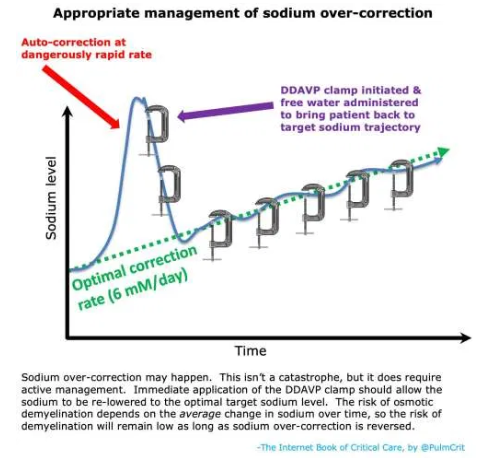
management of sodium over-correction
Over-correction will occasionally happen, even with proper management. That’s OK. With proper management, this can be rapidly fixed and patients will do fine.
risk factors for osmotic demyelination
- (1) Severe, chronic hyponatremia (especially a baseline sodium <110 mM)
- (2) High rate of sodium rise
- >8-10 mM per day on average may cause osmotic demyelination.
- If patients transition from chronic hyponatremia to hypernatremia, that’s the highest risk. Hypernatremia should be strongly avoided in patients who are recovering from hyponatremia.
- (3) Other patient-specific risk factors
- Cirrhosis
- Alcoholism
- Malnutrition
- Hypokalemia
key over-correction concept #1 = delayed deterioration
- Correction at rates >8-10 mM per day may cause osmotic demyelination syndrome (previously termed central pontine demyelination). This is a permanent, debilitating condition which must be avoided.
- Osmotic demyelination doesn’t occur immediately. So, if the patient over-corrects and still has a normal neurologic examination, this doesn’t mean that they couldn’t potentially develop osmotic demyelination soon.
- Even if the over-correcting patient looks OK, they’re still in trouble – and this still needs to be actively managed.
key over-correction concept #2 = you need to get back on track
Start here