Additional Resources
- Access the interactive tool here
- Read the Guideline At-a-Glance here
- Visit the guideline hub here
Today, I review excerpts from Section 2 Epidemiology and General Principals from ACC 2023 Chronic Choronary Disease Guideline.
2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Circulation. 2023 Aug 29;148(9):e9-e119. doi: 10.1161/CIR.0000000000001168. Epub 2023 Jul 20.
All that follows is from the above resource.
2 Epidemiology and General Principles
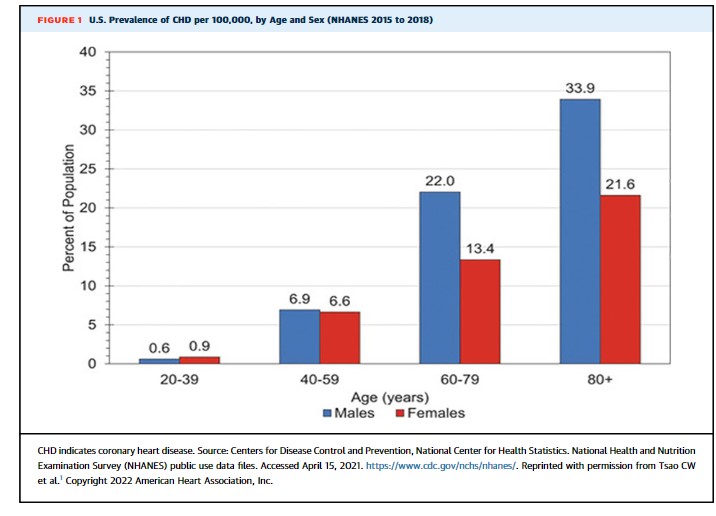
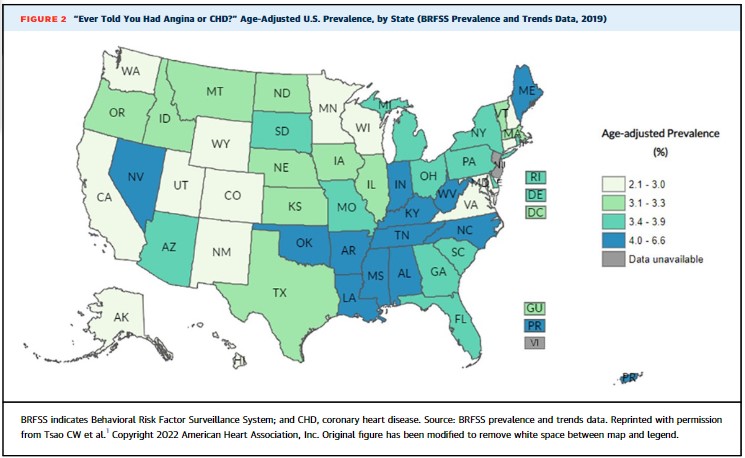
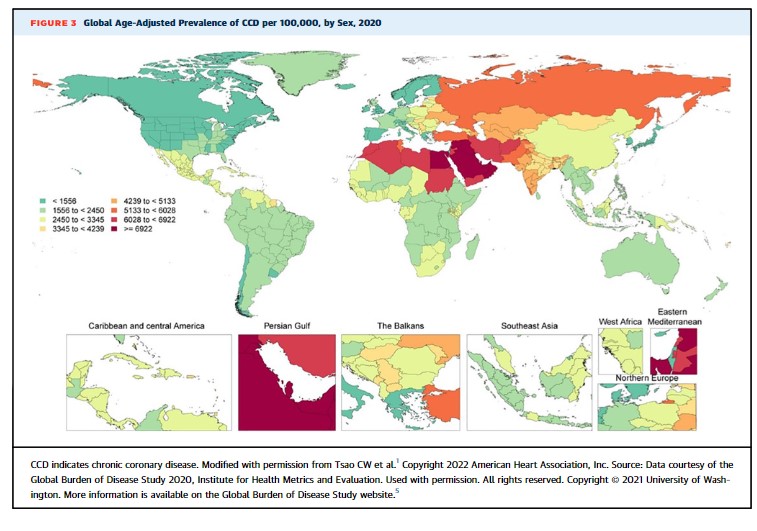
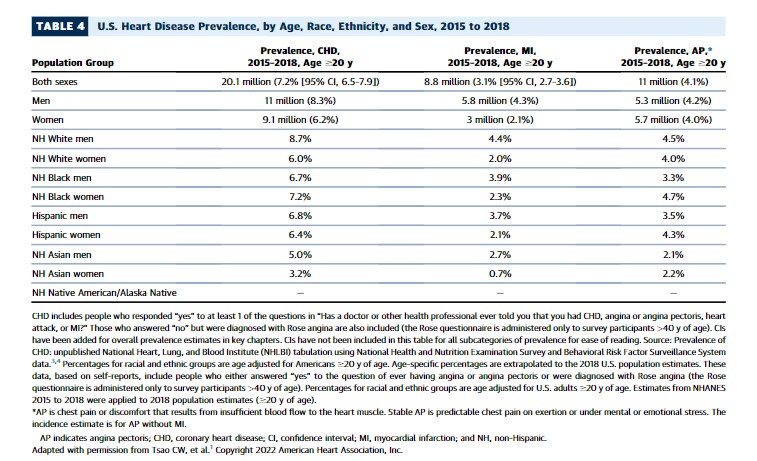
CCD is a heterogeneous group of conditions that includes obstructive and nonobstructive CAD with or without previous myocardial infarction (MI) or revascularization, ischemic heart disease diagnosed only by noninvasive testing, and chronic angina syndromes with varying underlying causes. Approximately 20.1 million persons in the United States live with CCD, 11.1 million Americans have chronic stable angina pectoris, and approximately one-quarter (n=200,000) of all MIs in the United States occur among the 8.8 million persons with CCD who have had a previous MI (Table 4).1 Despite an approximate 25% overall relative decline in death from coronary heart disease (CHD) over the past decade, it remains the leading cause of death in the United States and worldwide and is associated with substantial individual, economic, and societal burdens.1 Within the United States (Figures 1 and 2, Table 4) and worldwide (Figure 3), the prevalence of CCD and chronic stable angina vary by age, sex, race, ethnicity, and geographic region, and the role of SDOH in both risk for and outcomes from CCD is increasingly recognized.1
Since the publication of the “2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease,”2 not only have health care expenditures for CCD remained high, but also the number and complexity of comorbid conditions and concurrent treatments for those conditions among patients with CCD have increased. For example, older age and chronic kidney disease (CKD) commonly coexist with CCD and independently and together raise unique considerations for diagnosis, risk stratification, and treatment. At the intersection between CCD and atrial fibrillation (AF), new information informs the use of antiplatelet therapy and anticoagulation in patients with CCD and atrial fibrillation. Additionally, as the population ages and both CCD and cancer survival improve, concurrent CCD and cancer more often coexist, and the field of cardio-oncology has emerged to address the challenges of these intersecting chronic conditions. Further, the fields of diabetes and lipid management have evolved rapidly with multiple new therapies (eg, sodium glucose cotransporter 2 [SGLT2] inhibitors, glucagon-like peptide-1 [GLP-1] receptor agonists, proprotein convertase subtilisin/kexin type 9 [PCSK9] inhibitors, bempedoic acid, and inclisiran) emerging in these areas, and the range of diagnostic and interventional procedures available for use in patients with CCD has expanded. Thus, this guideline will address established diagnostic, risk stratification, and treatment approaches in a contemporary context, new therapies, and the intersection between CCD and other comorbid diseases in a framework that recognizes the importance of shared decision-making, team-based care, and cost and value.