Additional Resources
- Access the interactive tool here
- Read the Guideline At-a-Glance here
- Visit the guideline hub here
Today, I review excerpts from Section 1 Introduction from ACC 2023 Chronic Choronary Disease Guideline.
2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Circulation. 2023 Aug 29;148(9):e9-e119. doi: 10.1161/CIR.0000000000001168. Epub 2023 Jul 20.
All that follows is from the above resource.
1.1 Methodology and Evidence Review
The ACC and AHA have acknowledged the importance of value in health care to include development of cost–value statements for clinical practice recommendations. Available cost-effectiveness data were determined to be sufficient to support 9 specific recommendations in this guideline (Section 4.2.6, “Lipid Management”; Section 4.2.8, “SGLT2 Inhibitors and GLP-1 Receptor Agonists”; Section 5.1, “Revascularization”; and Section 8.1, “Cost and Value Considerations”). As a result, a Level of Value was assigned to those recommendations on the basis of the “ACC/AHA Statement on Cost/Value Methodology in Clinical Practice Guidelines and Performance Measures,”1 as shown in Table 1. Available quality-of-life (QOL) data were deemed to be insufficient to support specific recommendations in this guideline.
1.4 Scope of the Guideline
The scope of the “2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease” (referred to hereafter as the “2023 CCD guideline”) is to provide an update to and consolidate new evidence since the publication of the “2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease”3 and the “2014 ACC/AHA/AATS/PCNA/SCAI/STS Focused Update of the Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease” and will replace these prior guidelines.4 This current document provides a patient-centered approach to management of chronic coronary disease (CCD) incorporating the principles of shared decision-making, social determinants of health (SDOH), and team-based care. Where applicable and based on availability of cost-effectiveness data, value recommendations are also provided for clinicians.
The primary intended audience for this guideline is clinicians in primary care and cardiology specialty who care for patients with CCD in the outpatient setting. It aims to provide succinct recommendations in the domains of diagnostic evaluation, symptom relief, improvement in QOL, and reduction of future atherosclerotic cardiovascular disease (ASCVD)–related events and heart failure (HF) in patients with CCD. The recommendations provided in this guideline pertain to the chronic outpatient care of patients with CCD. Clinicians are referred to the relevant guidelines when evaluating patients with acute chest pain, ACS, or both.5-9 See Table 2 for other relevant guidelines.
1.4.1 CCD Definition
This guideline is intended to apply to the following categories of patients in the outpatient setting:
▪ Patients discharged after admission for an ACS event or after coronary revascularization procedure and after stabilization of all acute cardiovascular issues.
▪ Patients with left ventricular (LV) systolic dysfunction and known or suspected coronary artery disease (CAD) or those with established cardiomyopathy deemed to be of ischemic origin.
▪ Patients with stable angina symptoms (or ischemic equivalents such as dyspnea or arm pain with exertion) medically managed with or without positive results of an imaging test.
▪ Patients with angina symptoms and evidence of coronary vasospasm or microvascular angina.
▪ Patients diagnosed with CCD based solely on the results of a screening study (stress test, coronary computed tomography angiography [CTA]), and the treating clinician concludes that the patient has coronary disease.
This guideline is structured to address epidemiology and general principles in the management and transition of care in patients with CCD (Section 2, “Epidemiology/General Principles”). This is followed by evaluation of patients with CCD presenting with angina symptoms and risk stratification for future CVD events in patients with CCD (Section 3, “Evaluation, Diagnosis, and Risk Stratification”). Section 4, “Treatment” focuses on guiding principles in the management of patients with CCD (Section 4.1, “General Approach to Treatment Decisions”), overview of lifestyle and medical therapy (Section 4.2, “Guideline-Directed Management and Therapy”), and medical therapies to reduce cardiovascular events and manage symptoms (Section 4.3, “Medical Therapy to Prevent Cardiovascular Events and Manage Symptoms”) in patients with CCD. This is followed by key considerations in decision-making related to revascularization in patients with CCD (Section 5, “Revascularization”). Special populations with key considerations are discussed next (Section 6, “Special Populations”), followed by recommendations related to follow-up and monitoring of patients with CCD (Section 7, “Patient Follow-up: Monitoring and Managing Symptoms”). Cost and value considerations while treating patients with CCD and future research needs in patients with CCD are covered in Section 8 (“Other Important Considerations”). Where applicable, key recommendations from ACC/AHA guidelines and other scientific statements (Table 2) pertinent to outpatient management of patients with CCD are referenced and discussed. Readers should refer to these ACC/AHA guidelines and scientific statements for further details.
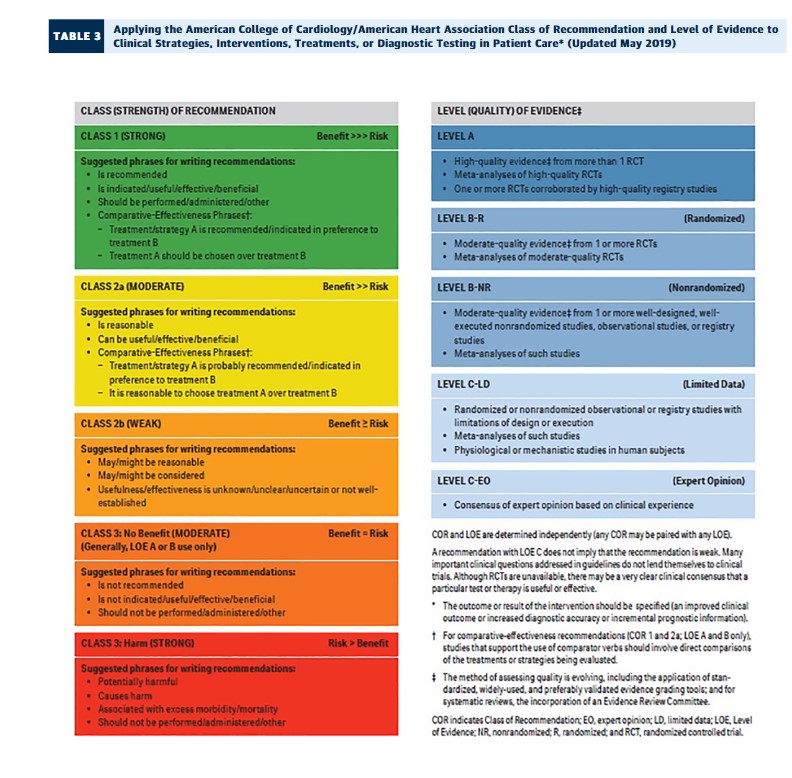
1.5 Class of Recommendations and Level of Evidence
The Class of Recommendation (COR) indicates the strength of recommendation, encompassing the estimated magnitude and certainty of benefit in proportion to risk. The Level of Evidence (LOE) rates the quality of scientific evidence supporting the intervention on the basis of the type, quantity, and consistency of data from clinical trials and other sources (Table 3).1